Patient Q&A with UNOS Chief Medical Officer David Klassen
Navigating the coronavirus pandemic is difficult for everyone, but brings special challenges for transplant patients. In a new video series on TransplantLiving.org, UNOS Chief Medical Officer David Klassen, M.D., answers questions for patients about COVID-19 and the waiting list, temporary inactivation, donor testing, living donation and other important topics.
Reactivation process for multiple kidney transplant candidates now available
As of April 22, kidney transplant programs are now able to simultaneously perform reactivation of multiple candidates whose current status is “Temporarily Inactive (7),” with inactive reason “COVID-19 Precaution.” Details and directions were sent via email to staff at all kidney transplant programs and posted on Secure Enterprise. In addition, step-by-step instructions are available in online help in UNetSM.
Programs also have the ability to perform temporary inactivation of multiple transplant candidates simultaneously for the reason of “COVID-19 Precaution,” which was released March 27. Together, this set of tools ensures offers are made efficiently to candidates who are immediately eligible for a transplant and streamlines the offer process.
Before temporarily inactivating candidates, please reference OPTN policy 3.6.A for information about whether candidates needing a particular organ type accrue waiting time while inactive.
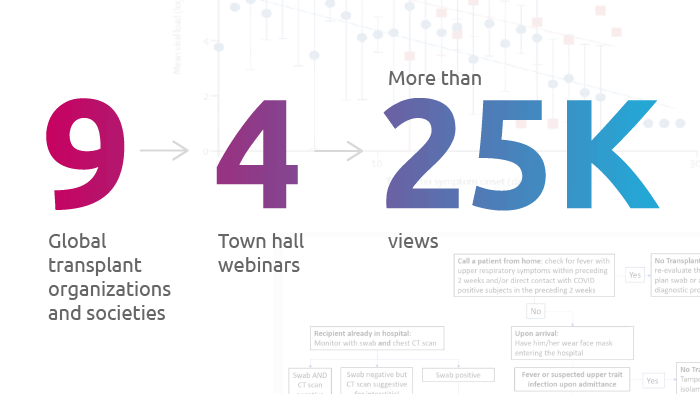
ISHLT presents new webinar: COVID-19 and challenges in advanced heart and lung disease and cardiothoracic transplantation
The International Society for Heart and Lung Transplantation is holding a free, live webinar for the cardiothoracic transplant community on April 29 at 4 p.m. ET. A recording will be posted for later viewing. Membership is not required and CE credit is available.
UNOS Staffing Survey deadline extended through Dec. 31
The deadline for the UNOS 2019 staffing survey has been extended from May 31 to Dec. 31. The extension is in response to the COVID-19 pandemic and will ensure maximum participation from as many hospitals as possible.
Reminders
COVID Collaborative now open for registration
The OPTN launched an interactive forum on April 22 so that members may engage on topics specific to donation and transplant during COVID-19. The OPTN COVID Collaborative operates on a secure online communication platform and allows donation and transplant professionals to collaboratively discuss, organize, catalog and archive the learnings and insights developed during the 2020 pandemic.
The site will:
- Offer discussion forums, facilitated by collaborative improvement specialists
- House and organize the member-driven information that results from this collaboration
- Be available for the duration of COVID-19, or until the decision is made to close the project
- Deploy national and regional webinars to support the spread of effective practices that emerge from site discussion
Participation in the COVID Collaborative is limited to individuals from OPTN member organizations. Registration is required. The scope of discussions will include OPTN member business and administrative processes related to the management of COVID crisis, and discussions will be moderated. Members with questions about policy during the pandemic should email member.questions@unos.org. Members with questions about policy compliance during the pandemic should email MQFeedback@unos.org.
Members may register here. Participants will receive an email with account and login information within two business days of registering.
For more information about the OPTN COVID Collaborative, email covidcollab@unos.org
Temporary changes to transplant program member monitoring as a result of the pandemic
MPSC leadership has evaluated specific areas of monitoring that are raising particular concern within the community. In an effort to encourage transplant programs to use their clinical judgement about what is in the best interests of their patients without the added concern of strict compliance with OPTN obligations, the MPSC will implement several time-limited emergency changes to member monitoring. These include:
- Suspending functional inactivity reviews through Sept. 30
- Placing a temporary hold on reviews of patient notification of extended waiting list inactivity and transplant program inactivation through Sept. 30
All time-limited COVID-related updates to monitoring changes may be found in a supplement to the OPTN member evaluation plan on the OPTN Compliance page. This document serves as a quick-reference guide to all member monitoring changes implemented as a result of the pandemic. It will be regularly updated with any additional monitoring changes implemented during this event.
Site surveys
Site surveys will be conducted virtually at least through the end of June. Any member who is not able to participate in a survey at this time can request a delay by emailing MQFeedback@UNOS.org
Patient safety portal reporting
Remember to report any suspected transplant-related disease transmissions through the Patient Safety Portal. At this time, the major transplant societies (AST, ASTS, AOPO, TTS) recommend against transplanting organs from a donor who has tested positive for COVID-19 from a respiratory tract sample or the blood, as this is likely indicative of an active infection that could be transmitted to a recipient, organ procurement team, transplant team or other contact.
New resources
Stay current
We will continue to update the UNOS COVID-19 resources page as guidance is developed and enhanced.
The post appeared first on UNOS.