Innovation: FEATURE
UNOS Labs is a collaborative space where scientists, researchers and technology experts partner with donation and transplantation professionals to develop new solutions aimed at increasing efficiency in the national transplant system and saving more lives.
UNOS LabsSM , an experimental incubator created in 2018, fills a critical role in bridging resources and research expertise to make innovation happen and bring big ideas to life. It enables our researchers to develop solutions to continuously improve the national organ donation and transplant system and increase organ utilization.
“We’ve begun this endeavor of UNOS Labs to address some of the bigger questions in transplant and try to meet the community where they are, and try and capitalize on a lot of the innovations that are out in the medical space,” said program manager Casey Humphries.
UNOS Labs explores and validates concepts and technologies that may be deployed across the nation’s organ transplant system. It is a place to try out new ideas under the primary pillars of behavioral research, data science and technology through extensive testing and incremental development.
“The emphasis in Labs is that projects have an end goal,” Humphries said. “They’re not academic, they’re not something that we want to just publish on and then store under the pillow. The goal of Labs is to create something that can be used to benefit the system.”
Improving the transplant system through innovation
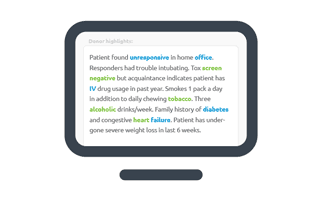
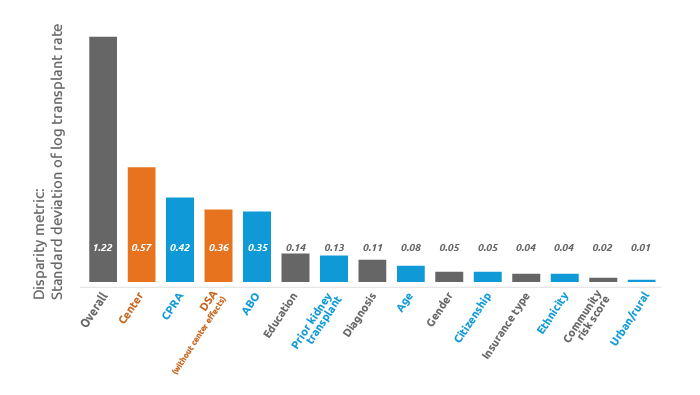
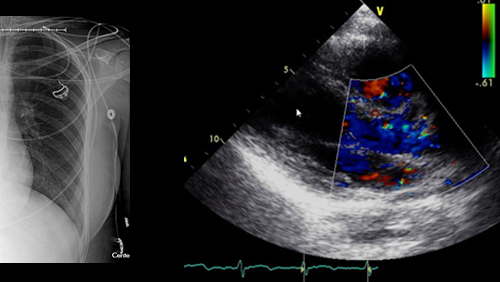
Among the new technologies UNOS researchers are leveraging is natural language processing (NLP) to predict which deceased donor kidneys will experience placement difficulties and to forecast which will be accepted by transplant hospitals. Encouraged by the study findings, the UNOS team plans to conduct more research to better understand the potential to enhance existing predictive models.
Humphries said a unique process such as NLP is a great example of data science.
“We have data science, and that’s really looking at understanding data broadly and looking at innovative ways to approach big data,” she said. “We can derive insights from using data science techniques…something that we can’t do with typical statistics.”
UNOS researchers are also partnering with organ procurement organizations (OPOs) nationwide to better predict organ travel time. One of the biggest contributors to prolonged cold ischemic time is coordinating logistics for organ transport. Using data gathered from couriers and pilot OPOs, researchers are also studying the feasibility of real-time tracking of organs shipped via ground and air.
Other partnership projects involving UNOS researchers include developing a series of simulation models to study the impact of possible changes to the transplant ecosystem; measuring physicians’ attitudes and perceptions around predictive analytics; and developing a liver paired exchange pilot program.
Philanthropic support for research and analytics
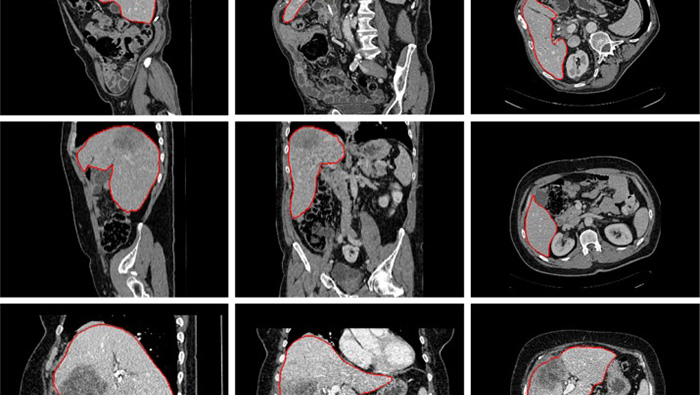
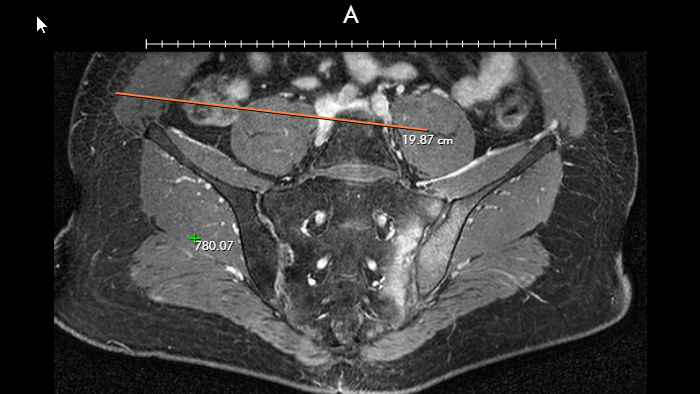
The Mendez National Institute of Transplantation Foundation recently awarded UNOS a $100,000 grant toward better understanding of the role biopsies play in transplant outcomes. The research further aims to improve the tools that inform kidney offer acceptance decisions.
The F.M. Kirby Foundation has given UNOS $75,000 to help train clinicians in promoting organ donation and increase the number of organ transplants during the COVID-19 pandemic. And the Fresenius Medical Care Foundation awarded UNOS $106,000 to help improve transportation and logistics for organ donation.
“We are challenging ourselves to think more broadly about the technologies we could bring to the transplant system,” explained Humphries. “Grants make this research happen.”
The post appeared first on UNOS.